COMPREHENSIVE APPROACHES TO DIAGNOSING AND MANAGING OBSTRUCTIVE SLEEP APNEA
Around 80 to 90 percent of adults with obstructive sleep apnea (OSA) remain undiagnosed, despite how common this condition is.1 OSA greatly affects a person’s quality of life and overall health. If left untreated, it can lead to other long-term health risks, such as heart disease, diabetes and more.
So, what can we do to prevent these patients from being overlooked? Let’s take a look at a detailed overview of OSA, including its definition, signs and symptoms, diagnostic approaches, and how inpatient OSA training, proactive screening and hospital-to-home care can help.
TRAINING OBJECTIVES
The primary goals of OSA overview are:
- Defining obstructive sleep apnea (OSA)
- Identifying the signs and risk factors of OSA
- Explaining diagnostic testing and physical examination approaches for OSA
- Understanding the importance of inpatient OSA training, proactive screening and hospital to home transitions
1. DEFINING AND IDENTIFYING OSA
a. What Is OSA?
Obstructive Sleep Apnea is a breathing disorder characterized by periodic cessation (apneas) or significantly diminished breathing (hypopneas) during sleep.1 These events lead to disrupted sleep and reduced oxygen levels, resulting in excessive daytime sleepiness and other health complications. OSA is typically diagnosed when an individual experiences five or more apneas or hypopneas per hour of sleep.1
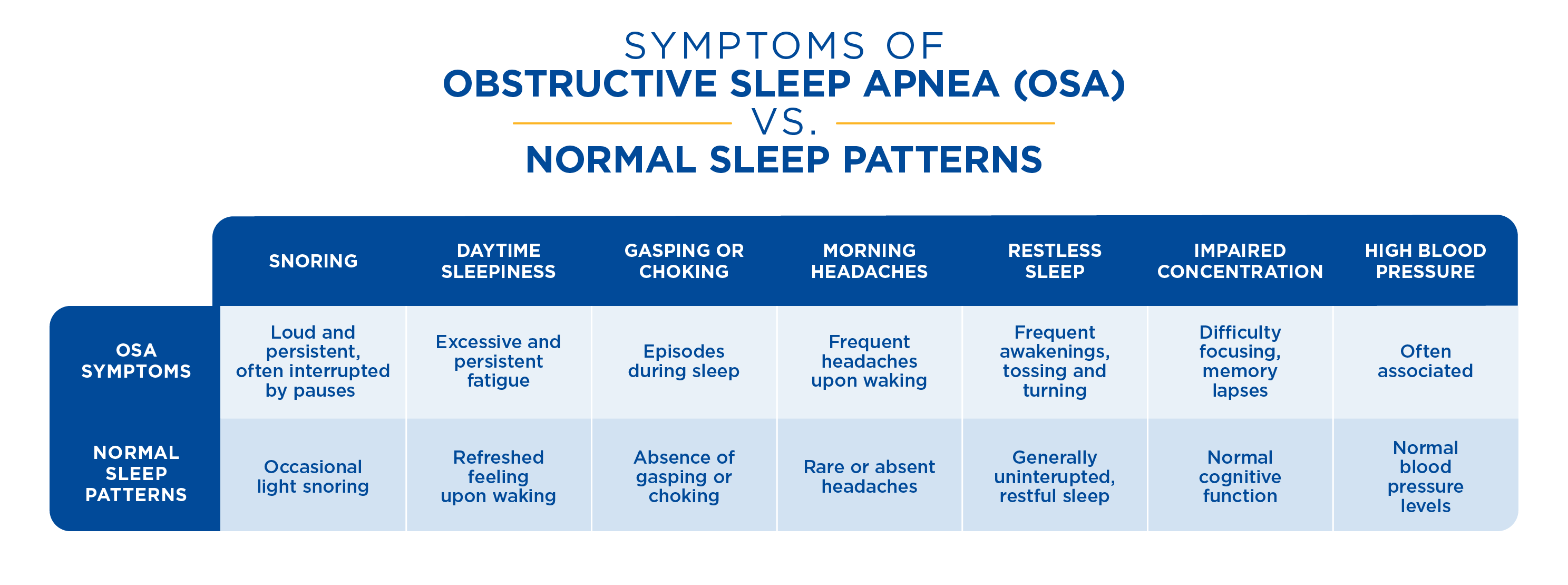
b. Symptoms of OSA
Patients with OSA often present with:2
- Excessive daytime sleepiness (EDS), struggling to stay awake during routine activities.
- Loud, disruptive snoring, frequently accompanied by silent intervals and gasps or snorts.
- Witnessed apneas, where breathing stops for several seconds during sleep, often reported by a bed
 partner.
partner. - Daytime fatigue, despite a full night’s sleep.
- Cognitive impairment, including difficulty concentrating, forgetfulness, and decreased alertness.
- Mood disturbances, such as irritability or depression.
- Sleep-related behaviors, like falling asleep during conversations or while driving.
- Unexplained chest pain during sleep that awakens the patient.
- Morning headaches upon waking, which are often due to low oxygen levels during sleep.
- Nocturia (frequent nighttime urination) and enuresis (bedwetting) can be associated with OSA.
2. SIGNS AND RISK FACTORS
a. Clinical Signs
Clinicians may observe:3
- Cyclical hypoxemia and hypercapnia: OSA leads to repeated cycles of low oxygen (hypoxemia) and high carbon dioxide (hypercapnia) levels in the blood during sleep.
- Cardiac arrhythmias: Irregular heart rhythms can occur due to intermittent hypoxemia and sleep fragmentation.
- Hypertension: Chronic OSA is a significant risk factor for high blood pressure, which can lead to cardiovascular disease.
b. Craniofacial Abnormality
Certain anatomical features can predispose individuals to OSA, such as:
- A small airway and disproportionate jaw structures, like retrognathia (receded jaw) and micrognathia (small jaw), can contribute to airway obstruction during sleep.4
c. Risk Factors
Risk factors for OSA include:2
- Overweight or obesity (BMI > 25 for overweight, > 30 for obese)
- Age (men 40+, women 50+)
- Family history of OSA
- Thick neck (men > 17 inches, women > 16 inches)
- Small airways in nose, throat, or mouth
- Excess soft tissue at the back of the throat or a larger-than-average tongue
- Smoking, which promotes inflammation and fluid retention in the upper airway
3. SCREENING AND DIAGNOSING OSA
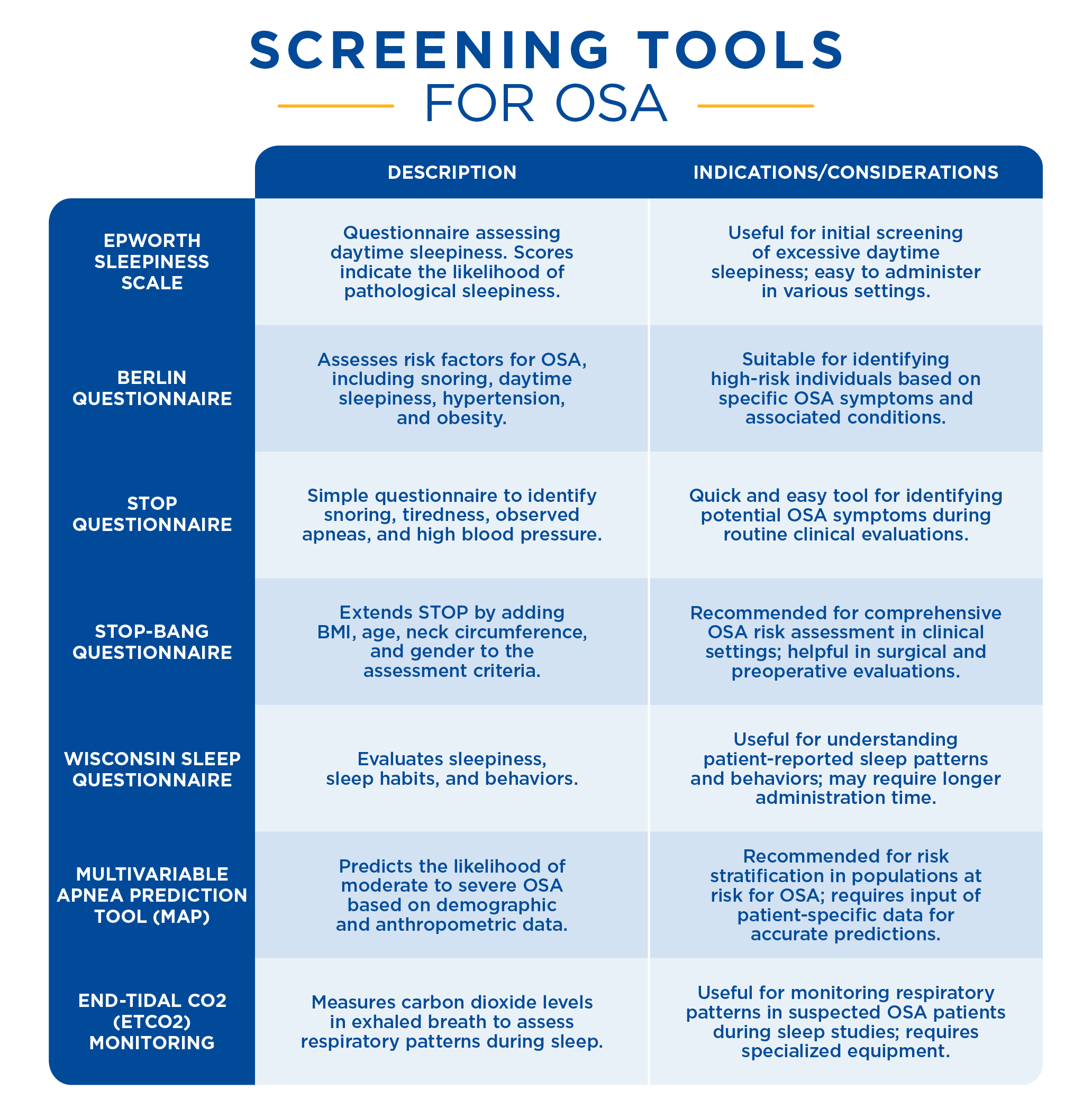
a. Screening Tools
Effective screening tools for OSA include:5
- Berlin Questionnaire: Assesses risk factors and symptoms to identify individuals at high risk for OSA.
- STOP Questionnaire: Screens for snoring, tiredness, observed apneas, and high blood pressure.
- STOP-Bang Questionnaire: An extended version of the STOP Questionnaire that includes additional factors like BMI, age, neck circumference, and gender.
- Wisconsin Sleep Questionnaire: Evaluates sleep patterns and disorders, including OSA.
- Multivariable Apnea Prediction Tool: Uses various predictors to estimate the probability of sleep apnea.
b. Physical Examination
Key considerations during a physical exam include:6
- Complaints of fatigue or unrefreshing sleep: Patients frequently report persistent tiredness despite adequate sleep duration.
- Newly diagnosed, resistant, or refractory hypertension: High blood pressure that does not respond well to treatment can be a sign of OSA.
- Congestive heart failure with nighttime chest pain: Cardiovascular issues exacerbated during sleep may indicate OSA.
- Bariatric patients: Individuals with severe obesity are at high risk for OSA.
- Large neck circumference: A large neck can signal excess tissue that may block the airway.
- Small jaw: Anatomical features such as a small jaw can contribute to airway obstruction.
- Diabetes: There is a strong association between OSA and metabolic disorders like diabetes.
c. Questions to Identify OSA
Healthcare providers should ask questions such as: 
- Do you fall asleep easily while watching TV, reading, or during other activities? This question helps gauge the extent of daytime sleepiness.
- How often do you wake feeling unrefreshed? Persistent unrefreshing sleep is a key symptom of OSA.
- Is your snoring louder than your talking? Loud snoring is a common indicator of OSA.
- Has your snoring or nighttime breathing bothered others? Bed partners often observe signs of OSA.
- Does anything unusual happen at night while you sleep? Unusual nocturnal behaviors can be symptomatic of OSA.
d. Diagnostic Testing
Diagnostic tests for OSA include:
- Polysomnography (PSG): An overnight sleep study that is considered the gold standard for diagnosing OSA. This test records various physiological parameters during sleep, including brain activity, eye movements, muscle activity, heart rhythm, breathing patterns, and oxygen levels. The data collected helps determine the presence and severity of sleep apnea.7
During polysomnography, patients stay overnight in a sleep lab where sensors monitor their sleep stages and cycles. The test provides comprehensive data that can help identify other sleep disorders, making it an invaluable tool for accurate diagnosis.7
- Home Sleep Testing (HST): This offers a convenient and cost-effective alternative to polysomnography for diagnosing OSA. HST involves the use of portable monitoring devices that patients can use in the comfort of their homes. These devices typically measure airflow, respiratory effort, heart rate, and oxygen saturation. HST is particularly useful for patients who cannot undergo in-lab sleep studies due to logistical or health reasons.8
HST provides a more comfortable and less intrusive option for patients, allowing for the collection of sleep data in a familiar environment. While it may not capture as much detailed information as polysomnography, it is highly effective in diagnosing moderate to severe OSA.8
4. PREVENTING UNDERDIAGNOSIS OF OSA
Three key strategies stand out as crucial in helping prevent the underdiagnosis of patients with OSA: OSA training, proactive screening, and smooth hospital-to-home transitions. Let’s take a look at how they can ensure that patients’ signs, symptoms and risk factors aren’t overlooked:
![]()
a. Inpatient OSA Training
Inpatient OSA training plays a crucial role in equipping healthcare professionals with the knowledge and skills to recognize, diagnose, and manage obstructive sleep apnea effectively. 9 By educating hospital staff on the signs, symptoms, and diagnostic protocols of OSA, we empower them to conduct thorough assessments and initiate timely interventions. This training ensures that OSA is not overlooked during hospital admissions, leading to earlier diagnosis and treatment.
![]()
b. Proactive Screening
Implementing routine screening protocols in primary care settings is equally essential. Healthcare providers can use proven tools such as the Epworth Sleepiness Scale and STOP-Bang Questionnaire to help identify individuals at risk for OSA before symptoms escalate. 10 This proactive screening enables timely evaluation, ensuring that patients receive appropriate referrals for diagnosis and treatment, thus preventing their signs and symptoms from going unnoticed.
![]()
c. Hospital to Home Transitions
Smooth transitions from hospital to home are critical in maintaining continuity of care for OSA patients. This involves educating patients about their condition, ensuring they understand and adhere to treatment plans, and providing ongoing support and monitoring. By empowering patients to manage their health outside clinical settings, healthcare teams can optimize treatment adherence and long-term outcomes.
HOW IT ALL TIES TOGETHER
Inpatient OSA training reduces underdiagnosis of OSA and improves patient outcomes. When healthcare providers are trained in OSA management, they can advocate for proactive screening practices, facilitate smoother transitions from hospital to home care, and provide ongoing support to patients. Ultimately, integrating OSA training into inpatient settings enhances healthcare delivery, promotes patient-centered care, and contributes to better overall health outcomes for individuals affected by this prevalent sleep disorder.
Sources:
- American Academy of Sleep Medicine. (n.d.). Obstructive Sleep Apnea. In American Academy of Sleep Medicine: Sleep Education. sleepapnea.pdf
- American Academy of Sleep Medicine. (2020, August). Obstructive Sleep Apnea (S. Khosla & I. Shaikh, Eds.). American Academy of Sleep Medicine Sleep Education. https://sleepeducation.org/sleep-disorders/obstructive-sleep-apnea/
- Acharya, R., Basnet, S., Tharu, B., Koirala, A., Dhital, R., Shrestha, P., Poudel, D., Ghimire, S., & Kafle, S. (2020). Obstructive Sleep Apnea: Risk Factor for Arrhythmias, Conduction Disorders, and Cardiac Arrest. Cureus, 12(8). https://doi.org/10.7759/cureus.9992
- Maresky, H. S., Klar, M. M., Tepper, J., Gavriel, H., Ziv Baran, T., Shapiro, C. M., & Tal, S. (2019). Mandibular width as a novel anthropometric measure for assessing obstructive sleep apnea risk. Medicine, 98(4). MD.0000000000014040
- Oktay Arslan, B., Ucar Hosgor, Z. Z., & Orman, M. N. (2020). Which Screening Questionnaire is Best for Predicting Obstructive Sleep Apnea in the Sleep Clinic Population Considering Age, Gender, and Comorbidities? Turkish Thoracic Journal, 21(6), 383–389. turkthoracj.2019.19024
- Mayo Clinic. (2019). Obstructive sleep apnea - Diagnosis and treatment - Mayo Clinic. Mayoclinic.org. https://www.mayoclinic.org/diseases-conditions/obstructive-sleep-apnea/diagnosis-treatment/drc-20352095
- Mayo Clinic. (2018). Polysomnography (sleep study) - Mayo Clinic. Mayoclinic.org. https://www.mayoclinic.org/tests-procedures/polysomnography/about/pac-20394877
- Johns Hopkins Medicine. (n.d.). What to Know About an At-Home Sleep Test. Www.hopkinsmedicine.org.
- Su, L., Chen, R., Luo, J., & Xiao, Y. (2022). Current medical education improves OSA-related knowledge but not confidence in residents: An underappreciated public health risk. Frontiers in Psychiatry, 13. fpsyt.2022.973884
- Feltner, C., Wallace, I. F., Aymes, S., Jennifer Cook Middleton, Hicks, K. L., Schwimmer, M., Baker, C., Balio, C. P., Moore, D., Voisin, C. E., & Jonas, D. E. (2022, November). Screening for Obstructive Sleep Apnea in Adults: An Evidence Review for the U.S. Preventive Services Task Force [Internet]. Nih.gov; Agency for Healthcare Research and Quality (US). books/NBK588761/

.png)



