RECOGNIZING AND ADDRESSING SLEEP APNEA IN WOMEN
Sleep apnea has long been thought of as a condition that primarily affects men. However, this assumption overlooks the fact that women are also significantly affected by this sleep disorder, albeit in different ways. Despite being a silent epidemic, its impact on women’s health can be profound, especially when left untreated. This article explores the gender differences in sleep apnea, the unique challenges in diagnosing the condition in women, and the importance of recognizing and addressing sleep apnea in women across different life stages.
UNDERSTANDING THE GENDER DIFFERENCES IN SLEEP APNEA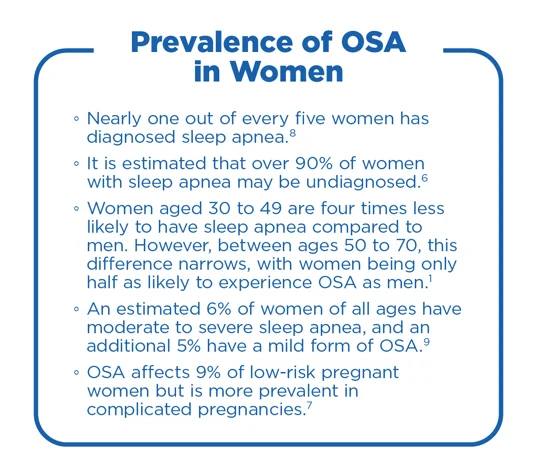
Historically, sleep apnea has been diagnosed more frequently in men than in women, leading to a misconception that it is a male-dominated condition. Studies indicate that men between the ages of 30 to 49 are four times more likely to have sleep apnea than women in the same age group. However, this likelihood decreases with age. Between the ages of 50 to 70, men are only twice as likely to experience OSA compared to women. This change is particularly notable after menopause, as the prevalence of sleep apnea in women increases, significantly narrowing the gender gap.1
This discrepancy has been partly attributed to the fact that men are more likely to exhibit the classic symptom of loud snoring, while women may present with subtler symptoms such as fatigue, insomnia, or mood disturbances.2 Anatomical differences, such as pharyngeal length and upper airway cross-sectional area, as well as hormonal influences, contribute to these gender disparities.3
The National Heart, Lung, and Blood Institute (NHLBI) also highlights that this gender difference in symptomatology often leads to a delay in diagnosis for women.4 Women are more likely to be misdiagnosed with other conditions like depression, anxiety, or insomnia before sleep apnea is considered.5
DIAGNOSING SLEEP APNEA IN WOMEN: DIAGNOSTIC CHALLENGES AND SOLUTIONS
One of the major challenges in diagnosing sleep apnea in women is that the symptoms often differ from those typically observed in men. While habitual snoring is a hallmark of sleep apnea, it may be absent in many women, leading to missed diagnoses. Women are more likely to present with symptoms such as insomnia (both sleep onset and maintenance), daytime fatigue, and restless legs syndrome (RLS), which are not as strongly associated with sleep apnea in the public consciousness.11
Common Symptoms in Women:6
Twenty percent of the general female population was found to be at high risk for obstructive sleep apnea. Among women at risk, the following symptoms were highly prevalent and reported:
- Habitual snoring (low risk: 19%, high risk: 61%)
- Sleep onset insomnia (32%)
- Maintenance insomnia symptoms (19%)
- Daytime sleepiness (24%)
- This symptom may also be absent in some cases
- Observed apnea (7%)
- Body movement (60%)
- Restless legs syndrome (RLS) symptoms (33%)
Source: (Kapsimalis & Kryger, 2009)
Symptoms of OSA can vary between men and women. Women may present with less typical symptoms such as insomnia or fatigue, rather than the more commonly recognized snoring and observed apneas. This variability is highlighted by the fact that only 61% of women at high risk for OSA exhibit habitual snoring, indicating that many do not.
Screening tools like the Berlin Questionnaire and STOP-Bang Questionnaire can help identify patients at risk of OSA. However, they may be less sensitive to the way sleep apnea manifests in women. Polysomnography remains the gold standard for diagnosis, but home sleep testing offers a convenient and effective alternative, especially for women who may be less inclined to undergo overnight sleep studies due to various barriers, including caregiving responsibilities and discomfort.
For a deeper dive into comprehensive strategies for diagnosing and managing sleep apnea, read our article, Bridging the Gap: Comprehensive Approaches to Diagnosing and Managing Obstructive Sleep Apnea. This resource offers valuable insights into best practices for healthcare providers aiming to improve patient outcomes through tailored approaches.
SLEEP APNEA IN WOMEN ACROSS DIFFERENT LIFE STAGES
Impact of Sleep Apnea on Young Women
Young women, especially those who are pregnant, face unique risks regarding sleep apnea. Pregnancy is associated with increased weight and changes in respiratory physiology, which can contribute to the development of OSA. Studies suggest that all pregnant women have an increased risk of developing sleep apnea, which can lead to adverse maternal and fetal outcomes, including gestational hypertension and preeclampsia, making early recognition and treatment essential.12
Screening Pregnant Women for Sleep Apnea
- Screening: If a pregnant woman presents with sleep issues, it is crucial to screen for sleep apnea. Utilize tools such as the Berlin Questionnaire or STOP-Bang Questionnaire to identify those at risk. Please note that these tools may be less sensitive to the way sleep apnea manifests in women.
- Home Sleep Apnea Testing (HSAT): Consider prescribing a home sleep apnea test (HSAT) for a more convenient and accessible diagnostic option, especially for pregnant women who may find it challenging to undergo overnight sleep studies.
- Alternative Therapies: For women diagnosed with sleep apnea during pregnancy, explore alternative therapies that are safe and effective during this period. Continuous Positive Airway Pressure (CPAP) therapy is commonly used, but other options may be considered based on individual needs.
- Postpartum Screening: After childbirth, reassess the patient’s sleep apnea status. Some women may experience a resolution of symptoms postpartum, while others may continue to require treatment
Sleep Apnea in Middle-Aged Women
As women enter middle age, the prevalence of sleep apnea increases, often coinciding with the onset of menopause. The hormonal changes associated with menopause, such as the decline in estrogen and progesterone, contribute to the development of sleep apnea by affecting airway muscle tone and respiratory function. Approximately 20% of women in the general population have sleep apnea.8 However, a significant portion of women is still undiagnosed.6 This is concerning, given the significant health risks associated with untreated sleep apnea, including cardiovascular disease and diabetes.
Postmenopausal Sleep Apnea: Understanding the Impact of Menopause on Sleep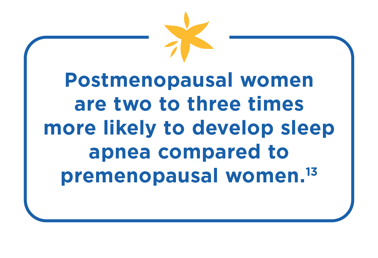
The link between menopause and sleep apnea is well-established. Menopause brings about several physiological changes that increase the risk of sleep apnea in women. The loss of progesterone and estrogen can cause the soft tissues in the throat to become more collapsible, increasing the risk of OSA. This hormonal shift, coupled with age-related changes such as weight gain and decreased muscle tone, makes postmenopausal women particularly vulnerable to OSA.5
As women transition into menopause, they often experience a worsening of sleep quality, characterized by frequent awakenings, night sweats, and insomnia. These sleep disturbances, in turn, can exacerbate OSA symptoms. Moreover, untreated sleep apnea in postmenopausal women is associated with serious health implications.4
Could It Be Sleep Apnea? Not Just Menopause Symptoms!
Menopause symptoms commonly linked to obstructive sleep apnea include:
Fatigue
Insomnia
Headaches

Night Sweats

Depression and Anxiety
Restless Leg Syndrome

Frequent Nighttime Urination

Weight Gain Due to Hormonal Changes
Health Implications of Untreated Sleep Apnea in Postmenopausal Women
The consequences of untreated sleep apnea in postmenopausal women are severe and associated with serious health implications.4 Untreated sleep apnea can significantly reduce quality of life and increase the likelihood of comorbid conditions, including:
- High blood pressure
- Heart disease
- Stroke
- Hypertension
- Diabetes
- Cognitive decline
- Mood disorders such as depression
Therefore, it is crucial for healthcare providers to screen for sleep apnea in postmenopausal women, especially those presenting with symptoms like hypertension or daytime fatigue.4
THE ROLE OF PATIENT EMPOWERMENT
Empowering women to recognize the symptoms of sleep apnea and seek appropriate treatment is essential in addressing this silent epidemic. Healthcare providers play a critical role in educating women about the risks of sleep apnea and encouraging them to speak up about their sleep concerns. By utilizing tailored screening questionnaires and promoting awareness, women can take proactive steps to manage their health. Patient empowerment also involves advocating for oneself when symptoms are dismissed or overlooked, ensuring that women receive the care they need.
CONCLUSION
Sleep apnea in women is a silent epidemic with far-reaching health implications. By understanding the gender-specific differences, addressing the diagnostic challenges, and focusing on patient empowerment, healthcare providers can better recognize and treat sleep apnea in women. With increased awareness and improved diagnostic tools, we can bridge the gap in diagnosis and treatment, leading to better health outcomes for women of all ages.
READY TO ENHANCE YOUR PRACTICE WITH
COMPREHENSIVE SLEEP CARE SOLUTIONS?
Apria offers tailored services designed to support the unique needs of women.
Partner with us to provide exceptional care and improve patient outcomes.
Sources
1. Peppard, P. E., Young, T., Barnet, J. H., Palta, M., Hagen, E. W., & Hla, K. M. (2013b). Increased Prevalence of Sleep-
Disordered Breathing in Adults. American Journal of Epidemiology, 177(9), 1006–1014. https://doi.org/10.1093/aje/kws342
2. Bryan, L., & Wells, A. (2024, March 19). How is Sleep Different for Men and Women? Sleep Foundation.
https://www.sleepfoundation.org/how-sleep-works/how-is-sleep-different-for-men-and-women
3. Badr, S. (2004, March 3). Gender Differences and Sleep Apnea. Sleep Review. https://sleepreviewmag.com/sleep-diagnostics/in-lab-tests/polysomnography/gender-differences-and-sleep-apnea/
4. National Heart, Lung and Blood Institute. (2020, January 13). Sleep apnea in women: New research could lead to better diagnosis and treatment | NHLBI, NIH. Www.nhlbi.nih.gov. https://www.nhlbi.nih.gov/news/2020/sleep-apnea-women-new-research-could-lead-better-diagnosis-and-treatment
5. Nox Medical. (2024, June 20). Sleep Apnea is Underdiagnosed in Women. Here’s Why. Nox Medical.
https://noxmedical.com/about/news-press/article/sleep-apnea-is-underdiagnosed-in-women-heres-why/
6. Kapsimalis, F., & Kryger, M. (2009). Sleep Breathing Disorders in the U.S. Female Population. Journal of Women’s
Health, 18(8), 1211–1219. https://doi.org/10.1089/jwh.2008.1054
7. Sanapo, L., Goldman, D., & Ghada Bourjeily. (2021). Obstructive sleep apnea in pregnancy: 1 sleep study may not be
enough in high-risk women. Journal of Clinical Sleep Medicine, 17(9), 1953–1956. https://doi.org/10.5664/jcsm.9340
8. The Society for Women’s Health Research. (n.d.). WOMEN & SLEEP APNEA. https://swhr.org/wp-content/uploads/2017/11/SWHR_Women-Sleep-Apnea.pdf
9. Breus, M. J. (2019). New Findings on Sleep Apnea in Women. Psychology Today.
https://www.psychologytoday.com/us/blog/sleep-newzzz/201906/new-findings-on-sleep-apnea-in-women
10. Singh, A., & Pacheco, D. (2023, June). Sleep Apnea Symptoms in Women | Sleep Foundation. Sleep Foundation.
https://www.sleepfoundation.org/sleep-apnea/sleep-apnea-symptoms-in-women#:~:text=Anywhere%20from%2010%25%20to%2015
11. Bonsignore, M. R., Saaresranta, T., & Riha, R. L. (2019). Sex differences in obstructive sleep apnoea. European
Respiratory Review, 28(154). https://doi.org/10.1183/16000617.0030-2019
12. Neurobit Health. (2023). Neurobit Research Blog | The Silent Epidemic: A New Study Unveils Obstructive Sleep Apnea’s Public Health Challenge. Neurobit.com. https://www.neurobit.com/blog/researchblogs/the-silent-epidemic-a-new-study-unveils-obstructive-sleep-apnea-s-public-health-challenge
13. Wilmer, S. (2024, January 25). Understanding the Link Between Menopause and Sleep Apnea - Sarah Wilmer DDS.
Sarah Wilmer DDS. https://www.sarahwilmerdds.com/blog/understanding-link-between-menopause-and-sleep-apnea/#:~:text=These%20changes%20can%20lead%20to
14. Lin, C. M., Davidson, T. M., & Ancoli-Israel, S. (2008). Gender differences in obstructive sleep apnea and treatment
implications. Sleep Medicine Reviews, 12(6), 481–496. https://doi.org/10.1016/j.smrv.2007.11.003

.png)



